At A Glance
- About 65 species of Demodex are known, but only two are responsible for Demodex blepharitis.
- Symptoms of Demodex blepharitis such as itching, burning, foreign body sensation, crusting, and tearing can resemble those of other ocular surface issues.
- Patients with Demodex blepharitis can be asymptomatic.
- Because of the overlap with symptoms and clinical presentation of dry eye, it is imperative to look for Demodex blepharitis on all patients.
The Demodex mite is the most common microscopic ectoparasite found on the human skin, specifically in or near the pilosebaceous unit, which consists of the hair, hair follicle, arrector pili muscle and sebaceous gland.1,2 About 65 species of Demodex are known, but only two, Demodex folliculorum and Demodex brevis, are responsible for Demodex blepharitis. In this article we take a closer look at educating patients about Demodex
SIGNS, SYMPTOMS, AND CLINICAL APPEARANCE
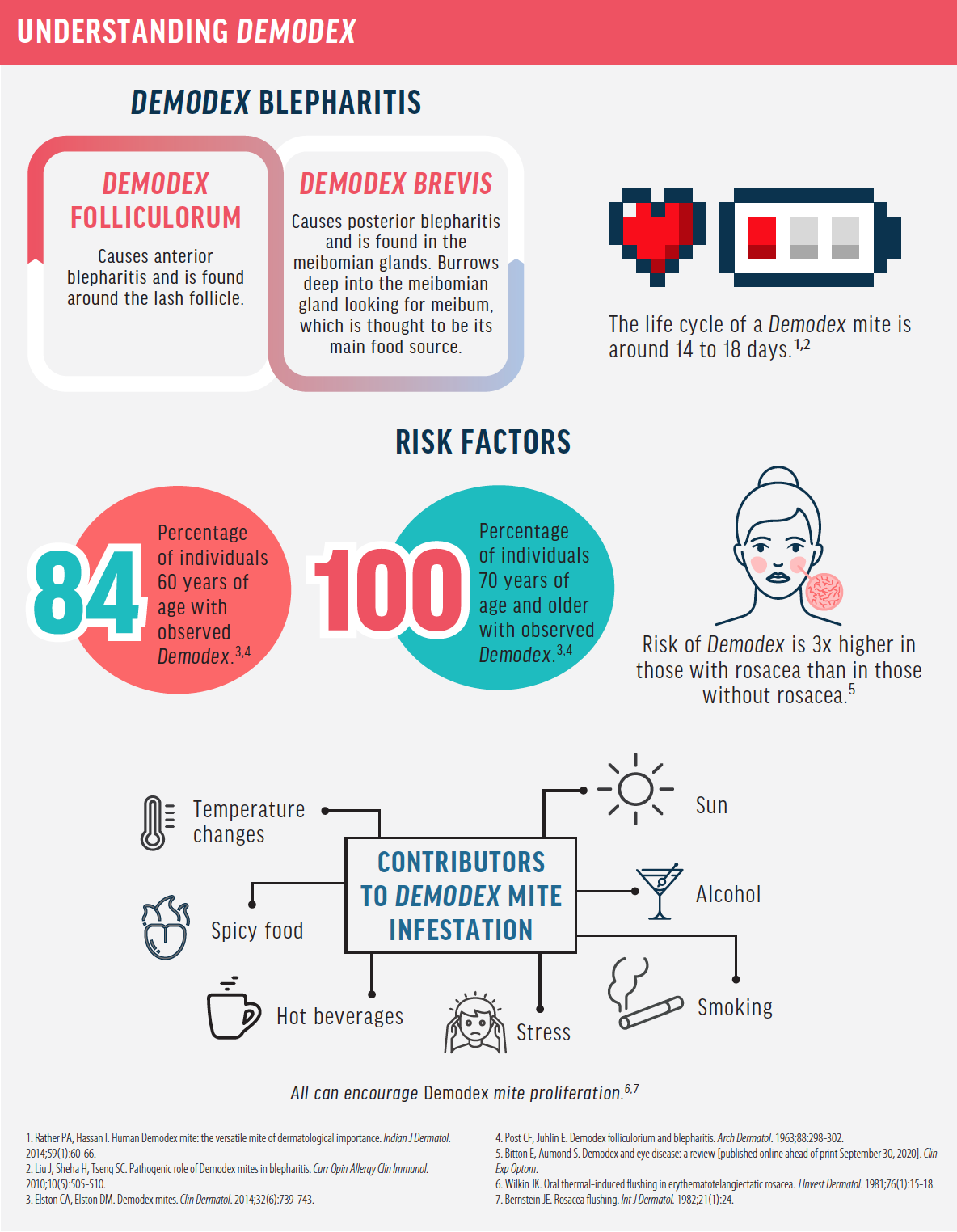
Demodex mites are tiny, ranging from 0.15 mm to 0.40 mm in length, making them nearly invisible to the naked eye.1 However, the presence of cylindrical dandruff, also known as collarettes, at the base of the eyelash is considered to be pathognomonic for the presence of Demodex folliculorum. This debris is present at the base of the eyelash follicle, where it remains as the lash grows. The wax-like dandruff is composed of Demodex mite remains and the hyperkeratinization caused by microabrasions from the mite’s claws.3 Collarettes are best observed on the superior eyelid while examining patients with their eyelids closed under slit-lamp magnification (Figure 1).
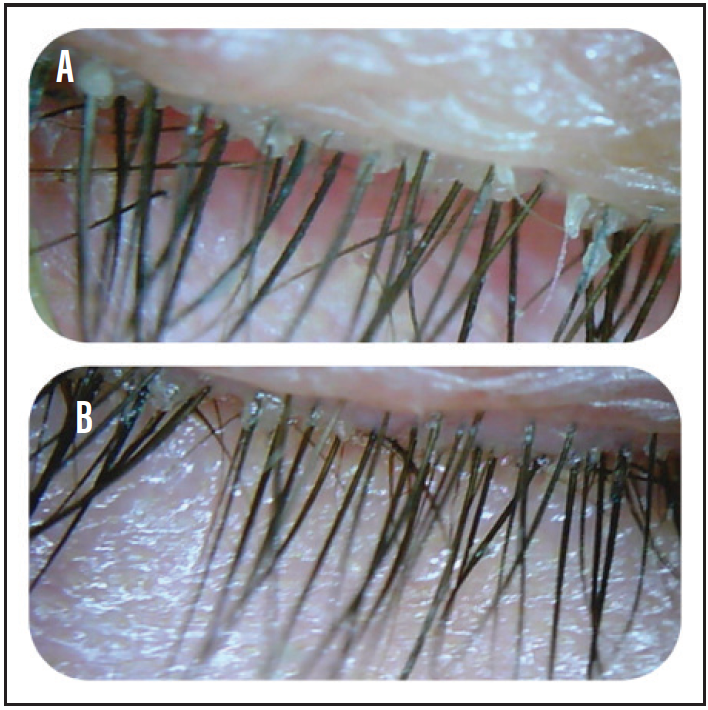
Figure 1. Significant presence of collarettes (A), a finding pathognomonic for Demodex infestation. The same patient after in-office microexfoliation using jojoba oil and a foam-based cleanser (B).
Other signs of Demodex infestation include meibomian gland dysfunction, lid margin erythema, follicular distention, lash loss, and misdirected lashes, as the infestation can alter the structure of the follicles. Symptoms can resemble those of many other ocular surface issues and can include itching, burning, foreign body sensation, crusting, tearing, blurry vision, discomfort, and irritation.
PATIENT MANAGEMENT CONSIDERATIONS
Because patients with Demodex blepharitis can often be asymptomatic, it is important to begin every clinical evaluation at the slit lamp with the patient’s eyes closed for a better view of the superior lid and lash margin, looking for the presence of collarettes.
Left untreated, the chronic inflammation associated with Demodex blepharitis can have many sequelae on the lid and the ocular surface, such as chronic hordeolum and chalazia. Chronic meibomian gland inflammation can lead to morphologic changes of the meibomian glands, gland atrophy, and meibomian gland dysfunction.4 Eyelid changes have also been noted with chronic inflammation, including lid margin telangiectasia, thickening of the lid margin, ocular rosacea, and even laxity of the eyelid over time. Chronic Demodex blepharitis is harmful to the follicles, leading to thinning and loss of eyelashes.
If inflammation persists, ocular surface involvement can be seen. Blepharoconjunctivitis is a common presentation.5 Demodex blepharitis should be considered in the presence of refractory recurrent blepharoconjunctivitis in the pediatric population.6 Demodex infestation may cause various sight-threatening corneal lesions including superficial corneal vascularization, marginal infiltration, a phlyctenule-like lesion, superficial opacity, and nodular scarring of the cornea.5,7 Due to the involvement of the cornea and conjunctiva with Demodex infestations, it is not uncommon to see contact lens intolerance in these patients.
As with all ocular conditions, it is important to educate patients about the findings of their examination. Demodex blepharitis, however, requires a complicated conversation. When presenting this diagnosis, it is best to normalize it to prevent psychosis and educate the patient that Demodex mites are a common finding on human skin (see Understanding Demodex).
Due to the overlap with the symptoms and clinical presentation of dry eye, it is imperative that we look for Demodex blepharitis on all patients. For some, a correct diagnosis will improve outcomes significantly when combined with dry eye treatment.
TREATMENT OPTIONS
Tea tree oil is an essential oil from the Melaleuca alternifolia plant that is known for its antiinflammatory and antiseptic properties. Tea tree oil has been found effective at reducing the number of Demodex mites and associated ocular surface inflammation in patients with Demodex blepharitis. Scientists have identified terpinen-4-ol (T40) as the most active ingredient in tea tree oil and isolated it for treatment of Demodex.8 Cliradex (Bio-Tissue), which contains a high concentration of T40, has been shown to effectively kill adult mites within 40 minutes of exposure.8,9
Laser in vivo confocal microscopy (IVCM) has been shown to be an effective, noninvasive tool for the detection of Demodex mites (Figure 2).10 A recent study used IVCM to detect mites and eggs in patients treated topically with T4O wipes or with a combination of topical T4O wipes and oral ivermectin. The researchers found that in both treatment groups there was a significant reduction in the mite population.10 There was also an increase in the prevalence of detectable Demodex eggs in both treatment groups,10 suggesting that a pulsed treatment may be most effective when using topical agents such as T4O.
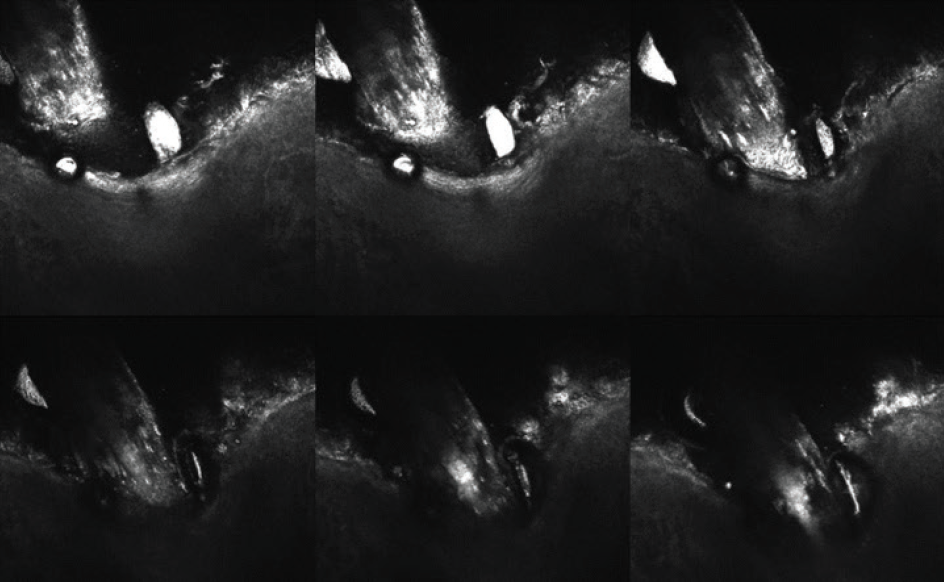
Figure 2. Image of an eyelash follicle using ICVM imaging. The bright white ovals near the lash follicle are Demodex eggs.
In-office treatment can be initiated with a microexfoliation procedure to begin the removal of collarettes. If this alone does not clear the lashes of collarettes, jojoba oil can be applied to the lash base with a cotton tip applicator and patients can be instructed to use T40 twice daily for 2 weeks. Typically, because of the 2-week life cycle of the Demodex mite, a return visit 2 weeks after initial treatment is recommended. In-office visits should be repeated biweekly until the mite count reaches zero based on the absence of clinical signs of collarettes.
Although T4O has been shown to be demodicidal, new research indicates that T4O, even at low levels, is toxic to human meibomian gland epithelial cells.11 Chen et al recently found a dose and time-dependent decrease in cell survival of human meibomian gland epithelial cells, with changes noted 15 minutes after exposure to 1% T4O and cell death after 90 minutes.11 These data confirm the need for evaluation of the meibomian gland structure and function prior to initiating any tea tree oil-based treatment and continued monitoring for changes over the treatment period. It may also spark us to look for alternative treatments.
Alternative Treatment Options
A few alternative treatments with limited evidence of safety and efficacy are available.
Manuka honey has antibacterial and antiinflammatory properties, and research shows it to be effective in treating the common comorbidity of Demodex blepharitis and rosacea.12 Optimel (Melcare Biomedical) is a topical Manuka honey eye drop that may have some effect on Demodex, but continued research is needed.
Fishman et al recently reported the effects of intense pulsed light on a Demodex mite extracted from a patient with ocular rosacea.13 Their results suggest that intense pulsed light application, with settings identical to those used for treatment of dry eye disease, causes complete destruction of the mite.
Another recent study suggests that the topical lid cleanser ZocuFoam (Zocular) may have demodicidal properties. The study authors concluded that, “ZocuFoam effectively killed Demodex significantly faster than preservative-free saline.”14 This okra-based cleanser killed Demodex about 91 minutes after exposure compared with the saline group at around 18 hours. Past studies have used mineral oil, which has a demodicidal rate similar to that of ZocuFoam, as a control. More research is needed before ZocuFoam would take the place of tea tree oil–based treatments.
TP-03 (Tarsus Pharmaceuticals) is a topical ophthalmic medication that targets the Demodex mite and has the potential to be the first prescription topical treatment for Demodex blepharitis. In the phase 2a SATURN-1 trial, treatment with TP-03 was effective, achieving collarette cure in 72% of patients and mite eradication in 78% of patients at day 42.15
AN ISSUE NOT TO BE IGNORED
Demodex is a common human parasite that can play an important role in contributing to ocular surface disease. Identifying these mites as the etiology of your patients’ symptoms can lead to profound improvements on their ocular surface. Demodex blepharitis is a growing concern, and our treatment options are limited.
- 1. Rather PA, Hassan I. Human Demodex mite: the versatile mite of dermatological importance. Indian J Dermatol. 2014;59(1):60-66.
- 2. Liu J, Sheha H, Tseng SC. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10(5):505-510.
- 3. Gao Y-Y, Di Pascuale MA, Li W, et al. High prevalence of ocular Demodex in lashes with cylindrical dandruffs. Invest Ophthalmol Vis Sci. 2005;46(9):3089-3094.
- 4. Cheng S, Zhang M, Chen H, Fan W, Huang Y. The correlation between the microstructure of meibomian glands and ocular Demodex infestation: A retrospective case-control study in a Chinese population. Medicine (Baltimore). 2019;98(19):e15595.
- 5. Kheirkhah A, Casas V, Li W, et al. Corneal manifestations of ocular Demodex infestation. Am J Ophthalmol. 2007;143(5):743-749.
- 6. Liu J, Sheha H, Tseng SC. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10(5):505-510.
- 7. Gao YY, Di Pascuale MA, Elizondo A, Tseng SC. Clinical treatment of ocular demodecosis by lid scrub with tea tree oil. Cornea. 2007;26(2):136-143.
- 8. Tighe S, Gao YY, Tseng SC. Terpinen-4-ol is the most active ingredient of tea tree oil to kill Demodex mites. Transl Vis Sci Technol. 2013;2(7):2.
- 9. Su CW, Tighe S, Sheha H, et al. Safety and efficacy of 4-terpineol against microorganisms associated with blepharitis and common ocular diseases. BMJ Open Ophthalmol. 2018;3(1):e000094.
- 10. Pondelis N, Hom MM, O’Dell LE, et al. Detection and assessment of treatment efficacy of Demodex blepharitis by in vivo confocal microscopy. Paper presented at: Association for Research in Vision and Ophthalmology Annual Meeting; April 29-May 3, 2018; Honolulu, Hawaii.
- 11. Chen D, Wang J, Sullivan DA, et al. Effects of terpin-4-ol on meibomian gland epithelial cells in vitro [published online ahead of print September 16, 2020]. Cornea.
- 12. Braithwaite I, Hunt A, Riley J, et al. Randomised controlled trial of topical kanuka honey for the treatment of rosacea. BMJ Open. 2015;5(6):e007651.
- 13. Fishman HA, Periman LM, Shah AA. Real-time video microscopy of in vitro Demodex death by intense pulsed light. Photobiomodul Photomed Laser Surg. 2020;38(8):472-476.
- 14. De Jesus M, Wong C, Yee RW (2106). Evaluation of the efficacy of ZocuFoam eyelid cleanser & moisturizer on the in vitro killing of ocular Demodex [White paper].
- 15. Tarsus releases data from lo and Europa trials for TP-03 to treat Demodex blepharitis and begins enrollment and treatment in phase 2b/3 Saturn-1 trial [press release]. PR Newswire. October 6, 2020. www.prnewswire.com/news-releases/tarsus-releases-data-from-io-and-europa-trials-for-tp-03-to-treat-demodex-blepharitis-and-begins-enrollment-and-treatment-in-phase-2b3-saturn-1-trial-301146578.html. Accessed October 16, 2020.